Tethered Spinal Cord Syndrome
Tethered Spinal Cord Syndrome
Tethered spinal cord syndrome is a neurological disorder caused by tissue attachments that limit the movement of the spinal cord within the spinal column. These attachments cause an abnormal stretching of the spinal cord. This syndrome is closely associated with spina bifida. It is estimated that 20 to 50 percent of children with spina bifida defects repaired shortly after birth will require surgery at some point to untether the spinal cord.
The lower tip of the spinal cord is normally located opposite the disc between the first and second lumbar vertebrae in the upper part of the lower back. In people with spina bifida (myelomeningocele), the spinal cord fails to separate from the skin of the back during development, preventing it from ascending normally, so the spinal cord is low-lying or tethered. In patients with a lipomyelomeningocele, the spinal cord will have fat at the tip and this may connect to the fat which overlies the thecal sac (a fluid filled sac that the spinal cord “floats” within.)
Although the skin is separated and closed at birth, the spinal cord stays in the same location after the closure. As the child continues to grow, the spinal cord can become stretched, causing damage and interfering with the blood supply to the spinal cord.
Primary Causes
In addition to myelomeningocele and lipomyelomeningocele discussed above, the following are other causes of tethered cord that vary in severity of symptoms and treatment.
- Dermal sinus tract (a rare congenital deformity)
- Diastematomyelia (split spinal cord)
- Lipoma (a benign, fatty growth)
- Tumor
- Thickened/tight filum terminale (a delicate filament near the tailbone)
- A history of spine trauma
- A history of spine surgery
Symptoms in Children
- Lesion on the lower back
- Fatty tumor or deep dimple on the lower back
- Skin discoloration on the lower back
- Hairy patch on the lower back
- Back pain, worsened by activity and relieved with rest
- Leg pain, especially in the back of legs
- Leg numbness or tingling
- Changes in leg strength
- Deterioration in gait
- Progressive or repeated muscle contractions
- Leg deformities
- Spine tenderness
- Scoliosis (curvature of the spine)
- Bowel and bladder problems
While fairly rare, this condition can continue undiagnosed into adulthood. In such cases, the strain on the spinal cord will increase, leading to increasing sensory and motor problems, as well as loss of bladder and bowel control.
Diagnosis
If a tethered cord is suspected, one or more tests may be necessary to confirm the diagnosis.
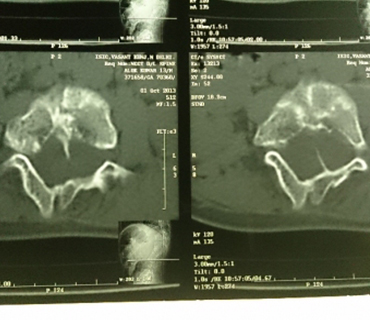
- Magnetic resonance imaging (MRI): A diagnostic test that produces three-dimensional images of body structures using powerful magnets and computer technology; can show the spinal cord, nerve roots, and surrounding areas, as well as enlargement, degeneration, and displacement.
- Myleogram: An x-ray of the spinal canal following injection of a contrast material into the thecal sac; can show pressure on the spinal cord or nerves due to tethered spinal cord.
- Computed tomography scan (CT or CAT scan): A diagnostic image created after a computer reads x-rays; may be used after a myelogram to show how the dye flows around the spinal cord and nerves.
- Ultrasound: A water-soluble gel is placed on the skin where the transducer (a handheld device that directs the high-frequency sound waves to the spine) is to be placed. The gel helps transmit the sound to your skin surface. The ultrasound is turned on and images of the spinal cord moving in the thecal sac are obtained.
Surgery
Untethering is generally performed only if there are clinical signs or symptoms of deterioration. The surgery involves opening the scar from the prior closure down to the covering (dura) over the myelomeningocele. Sometimes a small portion of the bony vertebrae (the laminae) are removed to obtain better exposure or to decompress the spinal cord. The dura is then opened, and the spinal cord and myelomeningocele are gently dissected away from the scarred attachments to the surrounding dura. Once the myelomeningocele is freed from all its scarred attachments, the dura and the wound are closed.
The child usually can resume normal activities within a few weeks. Recovery of lost muscle and bladder function depends upon the degree and length of preoperative implications. The combined complication rate of this surgery is usually only 1 to 2 percent. Complications include infection, bleeding, damage to the spinal cord or myelomeningocele, which may result in decreased muscle strength or bladder or bowel function. Many children require only one untethering procedure. However, since symptoms of tethering can occur during periods of growth, 10 to 20 percent require repeated surgery.