Spinal Cord Injury
Spinal Cord Injury
According to the National Spinal Cord Injury Association, as many as 450,000 people in the United States are living with a spinal cord injury (SCI). Most of these are caused by trauma to the vertebral column, thereby affecting the spinal cord’s ability to send and receive messages from the brain to the body’s systems that control sensory, motor and autonomic function below the level of injury.
Incidence
- The incidence of SCI is highest among persons age 16-30, in whom 53.1 percent of injuries occur; more injuries occur in this age group than in all other age groups combined.
- Males represent 81.2 percent of all reported SCIs and 89.8 percent of all sports-related SCIs.
- Among both genders, auto accidents, falls and gunshots are the three leading causes of SCI, in that order. Among males, diving accidents ranked fourth, followed by motorcycle accidents. Among females, medical/surgical complications ranked fourth, followed by diving accidents.
- Auto accidents are the leading cause of SCI in the United States for people age 65 and younger, while falls are the leading cause of SCI for people 65 and older.
- Sports and recreation-related SCI injuries primarily affect people under age 29.
The Spinal Cord
The spinal cord is about 18 inches long, extending from the base of the brain to near the waist. Many of the bundles of nerve fibers that make up the spinal cord itself contain upper motor neurons (UMNs). Spinal nerves that branch off the spinal cord at regular intervals in the neck and back contain lower motor neurons (LMNs). The spine itself is divided into four sections, not including the tailbone:
- Cervical vertebrae (1-7), located in the neck
- Thoracic vertebrae (1-12), in the upper back (attached to the ribcage)
- Lumbar vertebrae (1-5), in the lower back
- Sacral vertebrae (1-5), in the pelvis
Types and Levels of SCI
The severity of an injury depends on the part of the spinal cord that is affected. The higher the SCI on the vertebral column, or the closer it is to the brain, the more effect it has on how the body moves and what one can feel. More movement, feeling and voluntary control are generally present with injuries at lower levels.
- Tetraplegia (a.k.a. quadriplegia) results from injuries to the spinal cord in the cervical (neck) region, with associated loss of muscle strength in all four extremities.
- Paraplegia results from injuries to the spinal cord in the thoracic or lumbar areas, resulting in paralysis of the legs and lower part of the body.
Complete SCI
A complete SCI produces total loss of all motor and sensory function below the level of injury. Nearly 50 percent of all SCIs are complete. Both sides of the body are equally affected. Even with a complete SCI, the spinal cord is rarely cut or transected. More commonly, loss of function is caused by a contusion or bruise to the spinal cord or by compromise of blood flow to the injured part of the spinal cord.
Incomplete SCI
In an incomplete SCI, some function remains below the primary level of the injury. A person with an incomplete injury may be able to move one arm or leg more than the other, or may have more functioning on one side of the body than the other. An incomplete SCI often falls into one of several patterns.
Anterior cord syndrome results from injury to the motor and sensory pathways in the anterior parts of the spinal cord. These patients can feel some types of crude sensation via the intact pathways in the posterior part of the spinal cord, but movement and more detailed sensation are lost.
Central cord syndrome usually results from trauma and is associated with damage to the large nerve fibers that carry information directly from the cerebral cortex to the spinal cord. Symptoms may include paralysis and/or loss of fine control of movements in the arms and hands, with far less impairment of leg movements. Sensory loss below the site of the SCI and loss of bladder control may also occur, with the overall amount and type of functional loss related to the severity of damage to the nerves of the spinal cord.
Brown-Sequard syndrome is a rare spinal disorder that results from an injury to one side of the spinal cord. It is usually caused by an injury to the spine in the region of the neck or back. In many cases, some type of puncture wound in the neck or in the back that damages the spine may be the cause. Movement and some types of sensation are lost below the level of injury on the injured side. Pain and temperature sensation are lost on the side of the body opposite the injury because these pathways cross to the opposite side shortly after they enter the spinal cord.
Injuries to a specific nerve root may occur either by themselves or together with a SCI. Because each nerve root supplies motor and sensory function to a different part of the body, the symptoms produced by this injury depend upon the pattern of distribution of the specific nerve root involved.
“Spinal concussions” can also occur. These can be complete or incomplete, but spinal cord dysfunction is transient, generally resolving within one or two days. Football players are especially susceptible to spinal concussions and spinal cord contusions. The latter may produce neurological symptoms including numbness, tingling, electric shock-like sensations, and burning in the extremities. Fracture-dislocations with ligamentous tears may be present in this syndrome.
Penetrating SCI
“Open” or penetrating injuries to the spine and spinal cord, especially those caused by firearms, may present somewhat different challenges. Most gunshot wounds to the spine are stable, i.e., they do not carry as much risk of excessive and potentially dangerous motion of the injured parts of the spine. Depending upon the anatomy of the injury, the patient may need to be immobilized with a collar or brace for several weeks or months so that the parts of the spine that were fractured by the bullet may heal. In most cases, surgery to remove the bullet does not yield much benefit and may create additional risks, including infection, cerebrospinal fluid leak, and bleeding. However, occasional cases of gunshot wounds to the spine may require surgical decompression and/or fusion in an attempt to optimize patient outcome.
Diagnosis
When SCI is suspected, immediate medical attention is required. SCI is usually first diagnosed when the patient presents with loss of function below the level of injury.
Signs and Symptoms of Possible SCI
- Extreme pain or pressure in the neck, head or back
- Tingling or loss of sensation in the hand, fingers, feet, or toes
- Partial or complete loss of control over any part of the body
- Urinary or bowel urgency, incontinence, or retention
- Difficulty with balance and walking
- Abnormal band-like sensations in the thorax – pain, pressure
- Impaired breathing after injury
- Unusual lumps on the head or spine
Clinical Evaluation
A physician may decide that significant SCI does not exist simply by examining a patient who does not have any of the above symptoms, as long as the patient meets the following criteria: unaltered mental status, no neurological deficits, no intoxication from alcohol or other drugs or medications, and no other painful injuries that may divert his or her attention away from a SCI.
In other cases, such as when patients complain of neck pain, when they are not fully awake, or when they have obvious weakness or other signs of neurological injury, the cervical spine is kept in a rigid collar until appropriate radiological studies are completed.
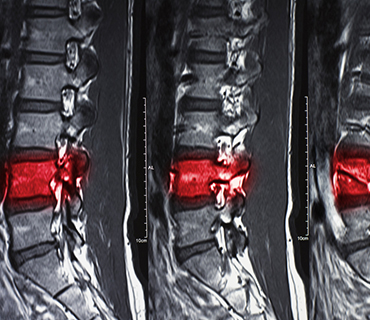
Radiological Evaluation
The radiological diagnosis of SCI has traditionally begun with x-rays. In many cases, the entire spine may be x-rayed. Patients with a SCI may also receive both computerized tomography (CT or CAT scan) and magnetic resonance imaging (MRI) of the spine. In some patients, centers may proceed directly to CT scanning as the initial radiological test. For patients with known or suspected injuries, MRI is helpful for looking at the actual spinal cord itself, as well as for detecting any blood clots, herniated discs, or other masses that may be compressing the spinal cord. CT scans may be helpful in visualizing the bony anatomy, including any fractures.
Even after all radiological tests have been performed, it may be advisable for a patient to wear a collar for a variable period of time. If patients are awake and alert but still complaining of neck pain, a physician may send them home in a collar, with plans to repeat x-rays in the near future, such as in one to two weeks. The concern in these cases is that muscle spasm caused by pain might be masking an abnormal alignment of the bones in the spinal column. Once this period of spasm passes, repeat x-rays may reveal abnormal alignment or excessive motion that was not visible immediately after the injury. In patients who are comatose, confused, or not fully cooperative for some other reason, adequate radiographic visualization of parts of the spine may be difficult. This is especially true of the bones at the very top of the cervical spine. In such cases, the physician may keep the patient in a collar until the patient is more cooperative. Alternatively, the physician may obtain other imaging studies to look for radiologically evident injury.
Treatment
Treatment of SCI begins before the patient is admitted to the hospital. Paramedics or other emergency medical services personnel carefully immobilize the entire spine at the scene of the accident. In the emergency department, this immobilization is continued while more immediate life-threatening problems are identified and addressed. If the patient must undergo emergency surgery because of trauma to the abdomen, chest, or another area, immobilization and alignment of the spine are maintained during the operation.
Intensive Care Unit Treatment
If a patient has a SCI, he or she will usually be admitted to an intensive care unit (ICU). For many injuries of the cervical spine, traction may be indicated to help bring the spine into proper alignment. Standard ICU care, including maintaining a stable blood pressure, monitoring cardiovascular function, ensuring adequate ventilation and lung function, and preventing and promptly treating infection and other complications, is essential so that SCI patients can achieve the best possible outcome.
Steroid Therapy
Methylprednisolone, a steroid drug, became available as a treatment for acute SCI in 1990 when a multicenter clinical trial showed better neurological change scores in patients who were given the drug within the first eight hours of injury. These studies have been criticized in part because this increase in scores has never been shown to translate into better functional outcomes for patients. This area remains controversial. Perhaps clinicians should consider methylprednisolone infusion if its potential benefits are felt to outweigh the risks of potential associated complications.
Surgery
Occasionally, a surgeon may wish to take a patient to the operating room immediately if the spinal cord appears to be compressed by a herniated disc, blood clot, or other lesion. This is most commonly done for patients with an incomplete SCI or with progressive neurological deterioration.
Even if surgery cannot reverse damage to the spinal cord, surgery may be needed to stabilize the spine to prevent future pain or deformity. The surgeon will decide which procedure will provide the greatest benefit to the patient.
Outcome
Persons with neurologically complete tetraplegia are at high risk for secondary medical complications. The percentages of complications for individuals with neurologically complete tetraplegia have been reported as follows:
- 3 percent developed pneumonia
- 8 percent developed pressure ulcers
- 4 percent developed deep vein thrombosis
- 2 percent developed a pulmonary embolism
- 2 percent developed a postoperative wound infection
Pressure ulcers are the most frequently observed complications, beginning at 15 percent during the first year postinjury and steadily increasing thereafter. The most common pressure ulcer location is the sacrum, the site of one third of all reported ulcers.
Neurological Improvement
Recovery of function depends upon the severity of the initial injury. Unfortunately, those who sustain a complete SCI are unlikely to regain function below the level of injury. However, if there is some degree of improvement, it usually evidences itself within the first few days after the accident.
Incomplete injuries usually show some degree of improvement over time, but this varies with the type of injury. Although full recovery may be unlikely in most cases, some patients may be able to improve at least enough to ambulate and to control bowel and bladder function. Patients with anterior cord syndrome tend to do poorly, but many of those with Brown-Sequard syndrome can expect to reach these goals. Patients with central cord syndrome often recover to the point of being ambulatory and controlling bowel and bladder function, but they often are not able to perform detailed or intricate work with their hands.
Once a patient is stabilized, care and treatment focuses on supportive care and rehabilitation. Family members, nurses, or specially trained aides all may provide supportive care. This care might include helping the patient bathe, dress, change positions to prevent bedsores, and other assistance.
Rehabilitation often includes physiotherapy, occupational therapy, and counseling for emotional support. The services may initially be provided while the patient is hospitalized. Following hospitalization, some patients are admitted to a rehabilitation facility. Other patients can continue rehab on an outpatient basis and/or at home.
Mortality
Mortality associated with SCI is influenced by several factors. Perhaps the most important of these is the severity of associated injuries. Because of the force that is required to fracture the spine, it is not uncommon for a SCI patient to suffer significant damage to the chest and/or abdomen. Many of these associated injuries can be fatal. In general, younger patients and those with incomplete injuries have a better prognosis than older patients and those with complete injuries.
Respiratory diseases are the leading cause of death in people with SCI, pneumonia accounting for 71.2 percent of these deaths. The second and third leading causes of death, respectively, are heart disease and infections.
Prevention
While recent advances in emergency care and rehabilitation allow many SCI patients to survive, methods for reducing the extent of injury and for restoring function are still limited. Currently, there is no cure for SCI. However, ongoing research to test surgical and drug therapies continues to make progress. Drug treatments, decompression surgery, nerve cell transplantation, nerve regeneration, stem cells, and complex drug therapies are all being examined in clinical trials as ways to overcome the effects of SCI. However, SCI prevention is crucial to decreasing the impact of these injuries on individual patients and on society.
Motor Vehicle Safety Tips
- Always wear a safety belt and make sure all passengers are wearing safety belts.
- Ensure that infants, toddlers and young children are properly restrained in an approved child safety seat that is installed correctly in the back seat.
- Ensure that all children 12 and younger ride in the back seat, properly restrained.
- Ensure that all children that have outgrown child safety seats are properly restrained in booster seats until they are age 8, or over 4’9″ tall.
- Obey speed limits and follow rules of the road at all times.
- Never drive under the influence of drugs or alcohol or ride as a passenger in a vehicle with a driver who is under the influence.
Tips to Prevent Falls in the Home
- Keep the floor clear and free of debris. Reduce clutter and move telephone and electrical cords out of walkways.
- Keep the floor clean, but do not apply floor wax. Clean up grease, water and other liquids immediately.
- Use non-skid throw rugs to reduce your chance of slipping on linoleum.
- Install handrails in stairways and grab bars in the bathroom (by toilets and in tub/shower.)
- Make sure living areas are well lit because it is easy to trip in the dark.
- Be aware that climbing and reaching high places will increase your chance of a fall. Use a sturdy step stool with hand rails when these tasks are necessary.
- Follow medication dosages closely. Using medication incorrectly may lead to dizziness, weakness and other side effects. These can all contribute to falls.
Water and Sports Safety Tips
- Do not dive in water less than 12 feet deep or in above-ground pools.
- Follow all rules at water parks and swimming pools.
- Do not participate in sports when you are ill or very tired.
- Wear proper safety gear approved for the specific sport.
- Avoid uneven or unpaved surfaces when cycling or skateboarding.
- Football players should receive adequate preconditioning and strengthening of the head and neck muscles.
- Proper football blocking and tackling techniques must be taught and followed.
- Check sports fields, playgrounds and equipment regularly for safety.
- Discard and replace sporting equipment or protective gear that is damaged.
Firearms Safety
- Always point the muzzle in a safe direction; never point a firearm at anyone or anything you don’t want to shoot.
- Keep your finger off the trigger and outside the trigger guard until you are ready to shoot.
- Keep the action open and the gun unloaded until you are ready to use it.
- Keep guns unloaded in a secure location so that children cannot access them.
- Store bullets in a separate, secure location so that children cannot access them.
- Explain to children that guns are dangerous and that they should never touch them, either at home or in any other environment, such as at friends’ houses.
- Talk with your teenager about ways to solve arguments without violence or guns.