Cerebral Aneurysm: Treatment Options
Cerebral Aneurysm: Treatment Options
What is an aneurysm?
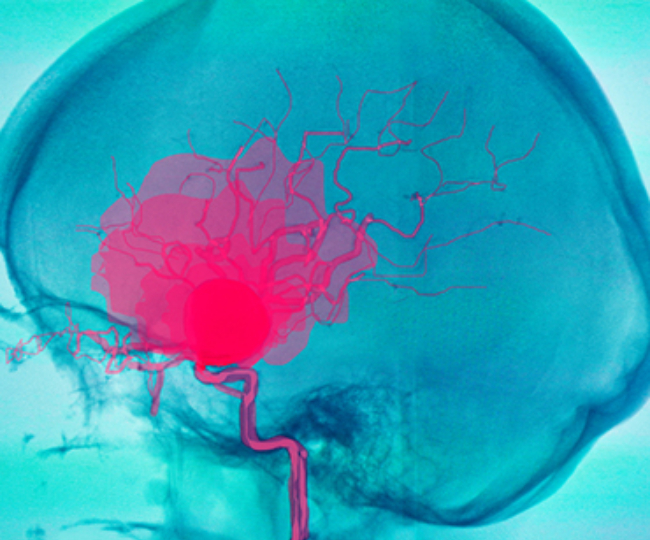
A cerebral or intracranial aneurysm is a dilation of an artery in the brain that results from a weakening of the inner muscular layer (the intima) of a blood vessel wall. The vessel develops a “blister-like” dilation that can become thin and rupture without warning. The resultant bleeding into the space around the brain is called a subarachnoid hemorrhage (SAH). This kind of hemorrhage can lead to a stroke, coma, and/or death.
The exact mechanisms by which cerebral aneurysms develop, grow, and rupture are unknown. However, a number of factors are believed to contribute to the formation of cerebral aneurysms. These include: 1) hypertension (high blood pressure); 2) cigarette smoking; 3) congenital (genetic) predisposition; 4) injury or trauma to blood vessels; 5) complication from some types of blood infections.
Types of Aneurysms:
An unruptured aneurysm is one whose sac has not previously leaked. An aneurysm ruptures when a hole develops in the sac of the aneurysm. The hole can be small, in which case only a small amount of blood leaks, or large, leading to a major hemorrhage. The management of both ruptured and unruptured cerebral aneurysms poses a significant challenge for patients and their treating physicians.
Treatment Options:
Today there are three treatment options for people with the diagnosis of cerebral aneurysm: 1) medical (non-surgical) therapy; 2) surgical therapy or clipping; and 3) endovascular therapy or coiling.
Medical Therapy:
Medical therapy is usually only an option for the treatment of unruptured intracranial aneurysms. Strategies include smoking cessation and blood pressure control. These are the only factors that have been shown to have a significant effect on aneurysm formation, growth, and/or rupture. Doctor may start you on an antihypertensive (blood pressure lowering) medication and/or diet and exercise program. Finally, periodic radiographic imaging conventional angiography may be recommended at intervals to monitor the size and/or growth of the aneurysm.
Surgical Clipping:
The mechanical sophistication of available clips, along with the advent of the operating microscope in the 1960s have made surgical clipping the gold standard in the treatment of both ruptured and unruptured cerebral aneurysms. In spite of these advances, surgical clipping remains an invasive and technically challenging procedure.
How is an aneurysm surgically clipped?
An aneurysm is clipped through a craniotomy, which is a surgical procedure in which the brain and the blood vessels are accessed through an opening in the skull. In the ideal clipping, normal blood vessel anatomy is physically restored by excluding the aneurysm sac from the cerebral circulation.
Endovascular Coiling:
Endovascular techniques for treating aneurysms uses the platinum detachable microcoil, which was used to treat the first human being in 1991. The development of Guglielmi detachable coils (GDCs) and their FDA approval in 1995, revolutionized endovascular treatment of cerebral aneurysms.
The common goal of both surgical clipping and endovascular coiling is to eliminate blood flow into the aneurysm. Efficacy (long-term success or effectiveness of the treatment) is measured by evidence of aneurysm obliteration (failure to be demonstrated by conventional or noninvasive angiography), without evidence of recanalization (any blood flow into the aneurysm) or recurrence (reappearance).
How is an aneurysm endovascularly coiled?
The microcatheter is selectively advance into the aneurysm itself, and the microcoils are released in a sequential manner. Once the coils are released into the aneurysm, the blood flow pattern within the aneurysm is altered, and the slow or sluggish remaining blood flow leads to a thrombosis (clot) of the aneurysm. A thrombosed aneurysm resists the entry of liquid blood, providing a seal in a manner similar to a clip.
Endovascular coiling is an attractive option for treating aneurysms because it does not require opening of the skull, and is generally accomplished in a shorter timeframe, which lessens the anesthesia given. Nevertheless, important differences remain between clipping and coiling, including the nature of the seal created. Because coiling does not physically reapproximate the inner blood vessel lining (endothelium), recanalization may occur through the eventual compaction of the coils into the aneurysm by the bloodstream.
The long-term durability of coiling is still unknown and not all aneurysms are suitable for coiling. As experience with coiling grows, the indications and pitfalls continue to be refined. Endovascular and coil technology continue to improve: endovascular adjuncts, such as intracranial stents, are now available to assist in coiling procedures; the original platinum microcoil has been refined with ever-improving features such as biological coating and microengineering for efficiency in deployment.
Who performs the procedure?
Surgical clipping of a cerebral aneurysm is always performed by a neurosurgeon, often one with expertise in cerebrovascular disease.
Endovascular coiling is done either by a neurosurgeon or by an interventional neuroradiologist.
How do I decide what procedure to have if I have a cerebral aneurysm?
The treatment of choice for an intracranial aneurysm, like all medical decisions, should be agreed upon by both the physician and the patient. In the case of either ruptured or unruptured intracranial aneurysms, the treating physician should discuss the risks and benefits of each available treatment option.