Adult Onset Hydrocephalus
Adult Onset Hydrocephalus
What Is Hydrocephalus?
The term hydrocephalus is derived from two words: “hydro,” meaning water, and “cephalus,” referring to the head.
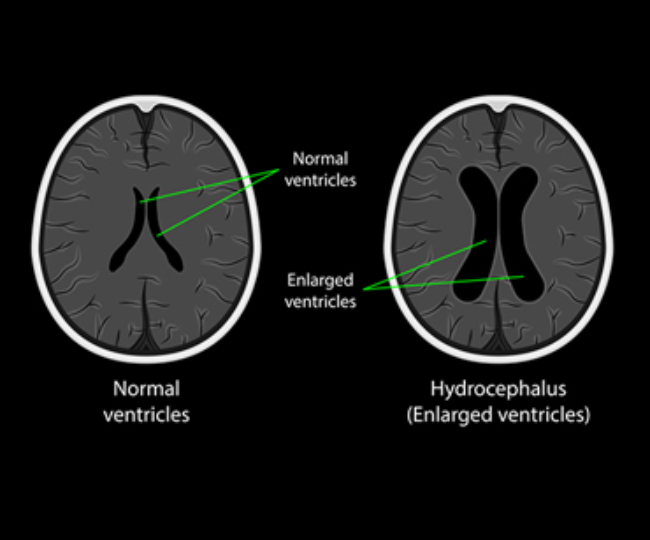
Hydrocephalus is a condition in which excess cerebrospinal fluid (CSF) builds up within the ventricles (fluid-containing cavities) of the brain and may increase pressure within the head. Although hydrocephalus often is described as “water on the brain,” the “water” actually is CSF — a clear fluid surrounding the brain and spinal cord.
CSF has three crucial functions: 1) it acts as a “shock absorber” for the brain and spinal cord; 2) it acts as a vehicle for delivering nutrients to the brain and removing waste; and 3) it flows between the cranium and spine to regulate changes in pressure within the brain.
The average adult produces about 475ml of CSF daily. When an injury or illness alters the circulation of CSF, one or more of the ventricles becomes enlarged as CSF accumulates. In an adult, the skull is rigid and cannot expand, so the pressure in the brain may increase profoundly.
Hydrocephalus can occur at any age, but is most common in infants and adults age 60 and older. It affects adult males and females, as well as people of different races, about equally. Experts believe that normal pressure hydrocephalus accounts for five to six percent of all dementia cases.
Hydrocephalus Ex-Vacuo
Hydrocephalus ex-vacuo occurs when a stroke or injury damages the brain and brain matter actually shrinks. The brain may shrink in older patients or those with Alzheimer’s disease, and CSF volume increases to fill the extra space. In these instances, the ventricles are enlarged, but the pressure usually is normal.
Normal Pressure Hydrocephalus (NPH)
Normal Pressure Hydrocephalus results from the gradual blockage of the CSF draining pathways in the brain. The ventricles enlarge to handle the increased volume of CSF, thus compressing the brain from within and eventually damaging or destroying the brain tissue. NPH owes its name to the fact that the ventricles inside the brain become enlarged with little or no increase in pressure. However, the name can be misleading, as some patients’ CSF pressure does fluctuate from high to normal to low when monitored.
NPH can occur as the result of head injury, cranial surgery, hemorrhage, meningitis or tumor. Unfortunately, the cause of the majority of NPH cases is unknown, making it difficult to diagnose and understand. Compounding this difficulty is the fact that some of the symptoms of NPH are similar to the effects of the aging process, as well as diseases such as Alzheimer’s and Parkinson’s. The majority of the NPH population is older than 60, and many of these people believe their symptoms are just part of the aging process. Unfortunately, many cases go unrecognized, are never properly treated or are misdiagnosed.
Symptoms of Adult-Onset Hydrocephalus
- Headaches
- Nausea
- Difficulty focusing the eyes
- Unsteady walk or gait
- Leg weakness
- Sudden falls
- Irritability
- Drowsiness
- Change in personality and behavior
- Seizures
Primary Symptoms of NPH
- Gait disturbance (difficulty walking)
- Dementia or forgetfulness
- Bladder control problems (as the condition progresses)
The symptoms of NPH usually get worse over time if the condition is left untreated. Patients with untreated, advanced NPH may experience seizures, which can get progressively worse. Dementia and/or bladder control problems usually appear after gait disturbances as the condition progresses. Mild dementia can be described as a loss of interest in daily activities, forgetfulness, difficulty dealing with routine tasks and short-term memory loss. Not everyone with NPH develops an obvious mental impairment.
Bladder control problems usually involve urinary frequency and urgency in mild cases. In severe cases, however, a complete loss of bladder control (urinary incontinence) may result. Urinary frequency is the need to urinate more than usual, often as frequently as every one to two hours. Urinary urgency is a strong, immediate physical need to urinate. This urge is sometimes so strong that it cannot be controlled, resulting in incontinence.
Diagnosing Hydrocephalus
Patients presenting the three primary NPH symptoms or a combination of the other symptoms should consult a neurosurgeon as soon as possible. Before your doctor can recommend a course of treatment, he or she will:
- Review your medical history and perform a physical examination
- Perform a complete neurological examination including diagnostic testing if needed
- Ask specific questions to determine if symptoms are caused by hydrocephalus
The neurological examination also will help to determine the severity of your condition. There are a wide variety of diagnostic tests that can help pinpoint the cause and severity of hydrocephalus.
Computed tomography scan (CT or CAT scan): A diagnostic image created after a computer reads X-rays; can show if the ventricles are enlarged or if there is an obvious blockage.
Magnetic resonance imaging (MRI): A diagnostic test that produces three-dimensional images of body structures using magnetic fields and computer technology; can evaluate the CSF flow and reveal if the ventricles are enlarged. The MRI provides more information than the CT scan, so it is the preferred test, in most cases.
Lumbar puncture (spinal tap): Under local anesthetic, a thin needle is passed into the spinal fluid space of the low back. Removal of up to 50 cc of CSF is done to see if symptoms are temporarily relieved. This test is used to measure CSF pressure and analyze the fluid. This procedure may help determine whether a shunt, the common treatment for hydrocephalus, will work. If lumbar puncture improves symptoms even temporarily, this can be an indication that a shunt will be successful. There are patients, however, who show no improvement and go on to have a successful shunt procedure.
When Surgery Is Necessary
Hydrocephalus can be treated in a variety of ways. The problem area may be treated directly (by removing the cause of CSF obstruction) or indirectly (by diverting the fluid to somewhere else, typically to another body cavity). Indirect treatment is performed by implanting a device known as a shunt to divert the excess CSF away from the brain. The body cavity in which the CSF is diverted usually is the peritoneal cavity (the area surrounding the abdominal organs).
Once inserted, the shunt system usually remains in place for the duration of a patient’s life, although additional operations to revise the shunt system may be needed. The shunt system continuously performs its function of diverting the CSF away from the brain, thereby keeping the intracranial pressure within normal limits.
An alternative operation called endoscopic third ventriculostomy may be recommended. In this operation, a tiny burr hole is made in the skull and a neuroendoscope (a small camera which is attached to medical instrument) is utilized to enter the brain. The neurosurgeon then will make a small hole (several millimeters) in the floor of the third ventricle, creating a new pathway through which CSF can flow.
Recovery
Your neurological function will be evaluated post-surgery. If any neurological problems persist, rehabilitation may be required to further your improvement. However, recovery may be limited by the extent of the damage already caused by the hydrocephalus and your brain’s ability to heal.
Because hydrocephalus is an ongoing condition, long-term follow-up by a doctor is required. Follow-up diagnostic tests, including CT scans, MRIs and X-rays, are helpful in determining if the shunt is working properly.
Prognosis
The prognosis for hydrocephalus depends on the cause, the extent of symptoms, and the timeliness of diagnosis and treatment. Some patients show a dramatic improvement with treatment, while others do not. In some instances of NPH, dementia can be reversed by shunt placement. Other symptoms such as headaches may disappear almost immediately if the symptoms are related to elevated pressure.
In general, the earlier hydrocephalus is diagnosed, the better the chance for successful treatment. The longer the symptoms have been present, the less likely it is that treatment will be successful.
Shunt malfunction or failure may occur.