Head Injury or Traumatic Brain Injury
Head Injury or Traumatic Brain Injury
A Head injury (HI) or traumatic brain injury (TBI) is defined as a blow to the head or a penetrating head injury that disrupts the normal function of the brain. HI can result when the head suddenly and violently hits an object, or when an object pierces the skull and enters brain tissue. Symptoms of a TBI can be mild, moderate, or severe, depending on the extent of damage to the brain. Mild cases may result in a brief change in mental state or consciousness, while severe cases may result in extended periods of unconsciousness, coma, or even death.
TBI Symptoms
Symptoms vary greatly depending on the severity of the head injury, but may include any of the following:
- Vomiting
- Lethargy
- Headache
- Confusion
- Paralysis
- Coma
- Loss of consciousness
- Dilated pupils
- Vision changes (blurred vision or seeing double, not able to tolerate bright light, loss of eye movement, blindness)
- Cerebrospinal fluid (CSF) (which may be clear or blood-tinged) coming out of the ears or nose
- Dizziness and balance problems
- Breathing problems
- Slow pulse
- Slow breathing rate, with an increase in blood pressure
- Ringing in the ears, or changes in hearing
- Cognitive difficulties
- Inappropriate emotional responses
- Speech difficulties (slurred speech, inability to understand and/or articulate words)
- Difficulty swallowing
- Body numbness or tingling
- Droopy eyelid or facial weakness
- Loss of bowel control or bladder control
If a TBI is suspected, immediately come to emergency or take the person to an emergency room.
Surgical Lesions
When discussing TBI, the term “mass lesion” is often used. This refers to an area of localized injury that may cause pressure within the brain. The most common mass lesions related to TBI are hematomas and contusions.
A hematoma is a blood clot within the brain or on its surface. Hematomas may occur anywhere within the brain. An epidural hematoma is a collection of blood between the dura mater (the protective covering of the brain) and the inside of the skull. A subdural hematoma is a collection of blood between the dura mater and the arachnoid layer, which sits directly on the surface of the brain.
A cerebral contusion is bruising of brain tissue. When examined under a microscope, cerebral contusions are comparable to bruises in other parts of the body. They consist of areas of injured or swollen brain mixed with blood that has leaked out of arteries, veins, or capillaries. Contusions are seen most commonly at the base of the front parts of the brain, but they may occur anywhere.
An intracerebral hemorrhage (ICH) describes bleeding within the brain tissue, which may be related to other brain injuries, especially contusions. The size and location of the hemorrhage helps determine whether it can be removed surgically.
Subarachnoid hemorrhage (SAH) is caused by bleeding into the subarachnoid space. It appears as diffuse blood spread thinly over the surface of the brain, and is seen commonly after TBI. Most cases of SAH associated with head trauma are mild. Hydrocephalus may result from severe traumatic SAH.
Diffuse Injuries
TBI can produce microscopic changes that cannot be seen on CT scans and that are scattered throughout the brain. This category of injuries is called diffuse brain injury, which may occur with or without an associated mass lesion.
Diffuse axonal injury refers to impaired function and gradual loss of some axons, which are the long extensions of a nerve cell that enable such cells to communicate with each other even if they are located in parts of the brain that are far apart. If enough axons are injured in this way, then the ability of nerve cells to communicate with each other and to integrate their function may be lost or greatly impaired, possibly leaving a patient with severe disabilities.
Another type of diffuse injury is ischemia, or insufficient blood supply to certain parts of the brain. This is crucial because a brain that has just undergone a traumatic injury is especially sensitive to even slight reductions in blood flow. Changes in blood pressure during the first few days after head injury can also have an adverse effect.
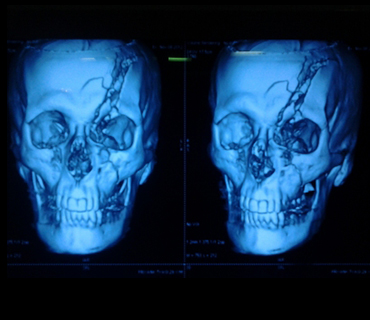
Skull Fractures
No treatment is required for most linear skull fractures, which are simple breaks or “cracks” in the skull. Of greater concern is the possibility that forces strong enough to cause a skull fracture may also have caused some damage to the underlying brain. Fractures of the base of the skull are problematic if they cause injury to nerves, arteries, or other structures. If a fracture extends into the sinuses, there may be leakage of cerebrospinal fluid (CSF) from the nose or ears. Most leaks will stop spontaneously.
Depressed skull fractures are those in which part of the bone presses on or into the brain. These may require surgical treatment. The damage caused by depressed skull fractures depends upon the region of the brain in which they are located and also upon the possible coexistence of any associated diffuse brain injury.
Diagnosis
The neurological examination includes an assessment utilizing the Glasgow Coma Scale (GCS).
Radiological Tests
A computed tomography scan (CT or CAT scan) is the gold standard for the radiological assessment of a TBI patient. A CT scan is easy to perform and is an excellent test for detecting the presence of blood and fractures, which are the most crucial lesions to identify in medical trauma cases.
Magnetic resonance imaging (MRI) is not commonly used for acute head injury, but MRI may demonstrate the existence of lesions that were not detected on the CT scan. This information is generally more useful for determining prognosis than for influencing treatment.
Surgical Treatment
In many cases, surgery is performed to remove a large hematoma or contusion that is significantly compressing the brain or raising the pressure within the skull. After surgery, these patients are usually observed and monitored in the intensive care unit (ICU).
Other head-injured patients may not go to the operating room immediately, but instead are taken from the emergency room to the ICU. Contusions or hematomas may enlarge over the first hours or days after head injury, so some patients are not taken to surgery until several days after an injury. On other occasions, a routine follow-up CT scan that was ordered to determine if a small lesion has changed in size indicates that the hematoma or contusion has enlarged significantly.
Medical Treatment
At the present time, there is no medication or “miracle treatment” that can be given to prevent nerve damage or promote nerve healing after TBI. The primary goal in the ICU is to prevent any secondary injury to the brain. Likewise, increases in ICP, decreases in blood oxygenation, increases in body temperature, increases in blood glucose, and many other disturbances can potentially worsen neurological damage. The prevention of secondary insults is a major part of the ICU management of head-injured patients.
Outcome
One of the most widely used systems to classify outcome from head injury is the Glasgow Outcome Scale (GOS). Patients with mild head injury (usually defined as GCS score on admission of 13-15) tend to do well. They may experience headaches, dizziness, irritability, or similar symptoms, but these gradually improve in most cases.
Patients with moderate head injuries fare less well. Approximately 60 percent will make a positive recovery, and an estimated 25 percent will be left with a moderate degree of disability. Death or a persistent vegetative state will be the outcome in about 7 to 10 percent of cases. The remainder of patients will have a severe degree of disability.
The group comprised of severely head-injured patients has the worst outcomes. Only 25 to 33 percent of these patients have positive outcomes. Moderate disability and severe disability each occur in about a sixth of patients, with moderate disability being slightly more common. About 33 percent of these patients do not survive. The remaining few percent remain persistently vegetative.
The above statistics apply to patients with so-called closed head injuries. For penetrating head injuries, which today are caused most commonly by handguns, outcomes follow a different pattern. More than 50 percent of all patients with gunshot wounds to the head who are alive upon arrival at a hospital do not survive because their initial injuries are so severe. However, most of the remaining patients tend to do fairly well, largely because their injuries are relatively mild (GCS score of 13-15). Relatively few patients suffer injuries of intermediate severity (GCS score of 9-12) from gunshot wounds, but it is this group that has the most variability in outcomes.
Rehabilitation
Once head-injured patients leave the acute-care hospital, some may benefit from a rehabilitation program. Prime candidates for rehabilitation are patients that had less severe initial injuries, or those that have started to show significant improvement. For more severely injured patients or for those whose recovery is slow, constant vigilance is required to prevent the gradual onset of problems with joint mobility, skin integrity, respiratory status, infection, and many other physiological functions. Patients with moderate or mild injuries, as well as severely injured patients who have improved sufficiently, may be candidates for outpatient therapy.
Regardless of the setting, most head-injury rehabilitation centers emphasize compensatory strategies, which essentially help patients learn to reach the maximum level of function allowed by their impairments. The concept of cognitive retraining, which presumes that at least some of the brain’s cognitive capacity can be restored by constant repetition of certain simple tasks, is more controversial but is also emphasized at many centers. Another major goal of head injury rehabilitation is working with patients’ families to educate them about what they can realistically expect and how they can best help their injured family member.
General Head Injury Prevention Tips
- Wear a helmet every time you drive or ride in a motor-cycle or two wheeler.
- Wear a seatbelt every time you drive or ride in a motor vehicle.
- Never drive while under the influence of drugs or alcohol or ride as a passenger with anybody else who is under the influence.
- Keep firearms unloaded in a locked cabinet or safe, and store ammunition in a separate, secure location.
- Remove hazards in the home that may contribute to falls. Secure rugs and loose electrical cords, put away toys, use safety gates, and install window guards. Install grab bars and handrails if you are frail or elderly.
Sports and Recreation Head Injury Prevention Tips
- Buy and use helmets or protective head gear approved by the ASTM for specific sports 100 percent of the time.
- Supervise younger children at all times, and do not let them use sporting equipment or play sports unsuitable for their age. Do not let them use playgrounds with hard surface grounds.
- Follow all rules and warning signs at water parks, swimming pools, and public beaches.
- Do not dive in water less than 12 feet deep or in above-ground pools. Check the depth – and check for debris in the water before diving.
- Wear appropriate clothing for the sport.
- Do not wear any clothing that can interfere with your vision.
- Do not participate in sports when you are ill or very tired.
- Obey all traffic signals and be aware of drivers when cycling or skateboarding.
- Avoid uneven or unpaved surfaces when cycling, skateboarding, or in-line skating.
- Perform regular safety checks of sports fields, playgrounds and equipment.
- Discard and replace sporting equipment or protective gear that is damaged.
- Never slide head-first when stealing a base.